The EPIC-CAD trial, recently published in The New England Journal of Medicine, evaluated the efficacy and safety of edoxaban monotherapy compared to dual antithrombotic therapy in patients with stable coronary artery disease (CAD) and high-risk atrial fibrillation (AF). This open-label, … Read More
atrial fibrillation
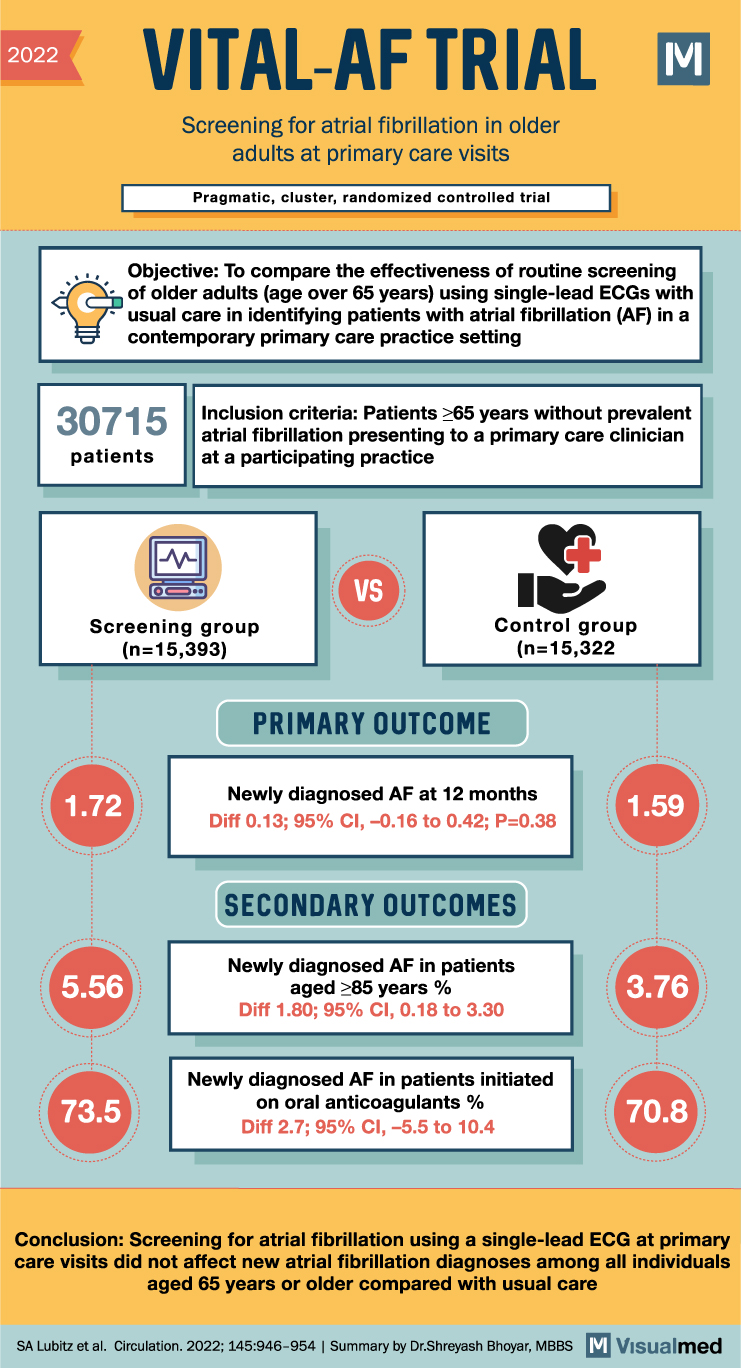
VITAL-AF Trial: Screening for AFib
VITAL-AF Trial Summary The VITAL-AF trial aimed to determine whether point-of-care screening with a handheld single-lead ECG device during primary care visits increases the diagnosis of atrial fibrillation (AF) in older adults. The study randomized 16 primary care clinics in … Read More
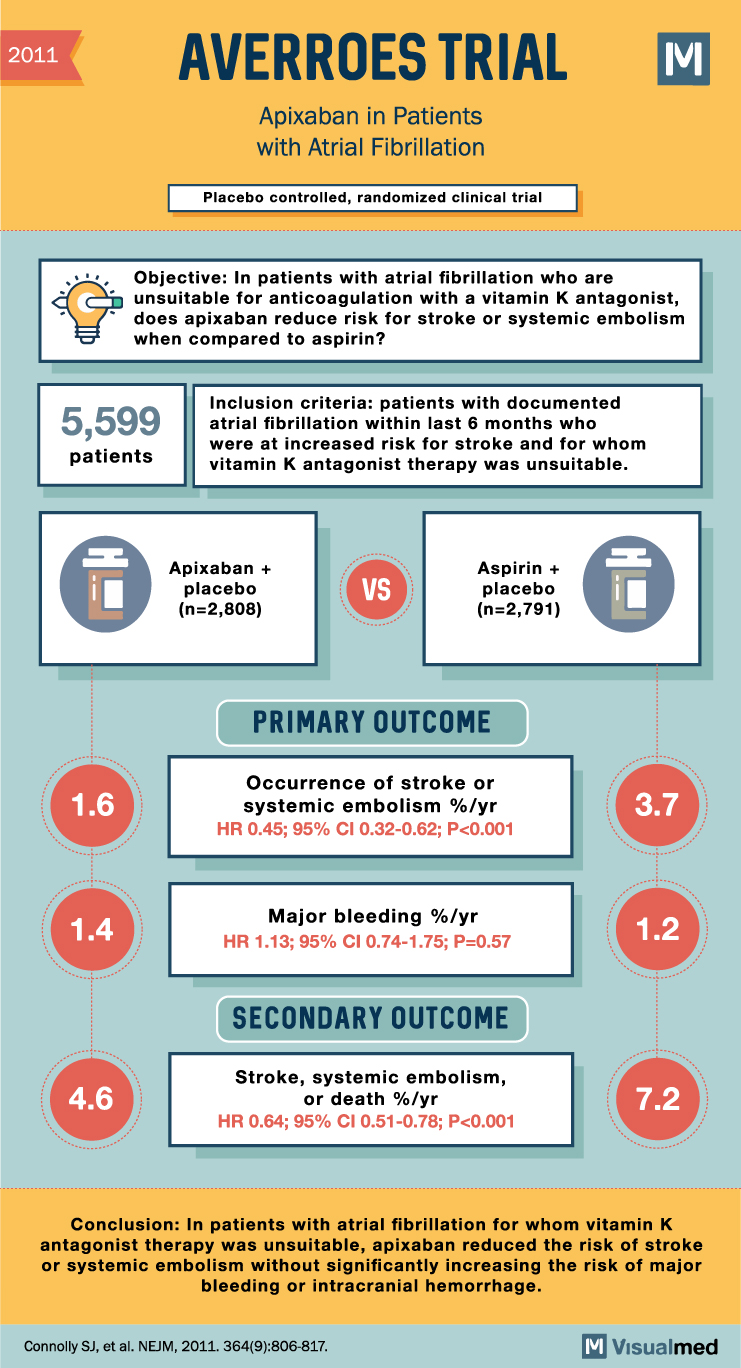
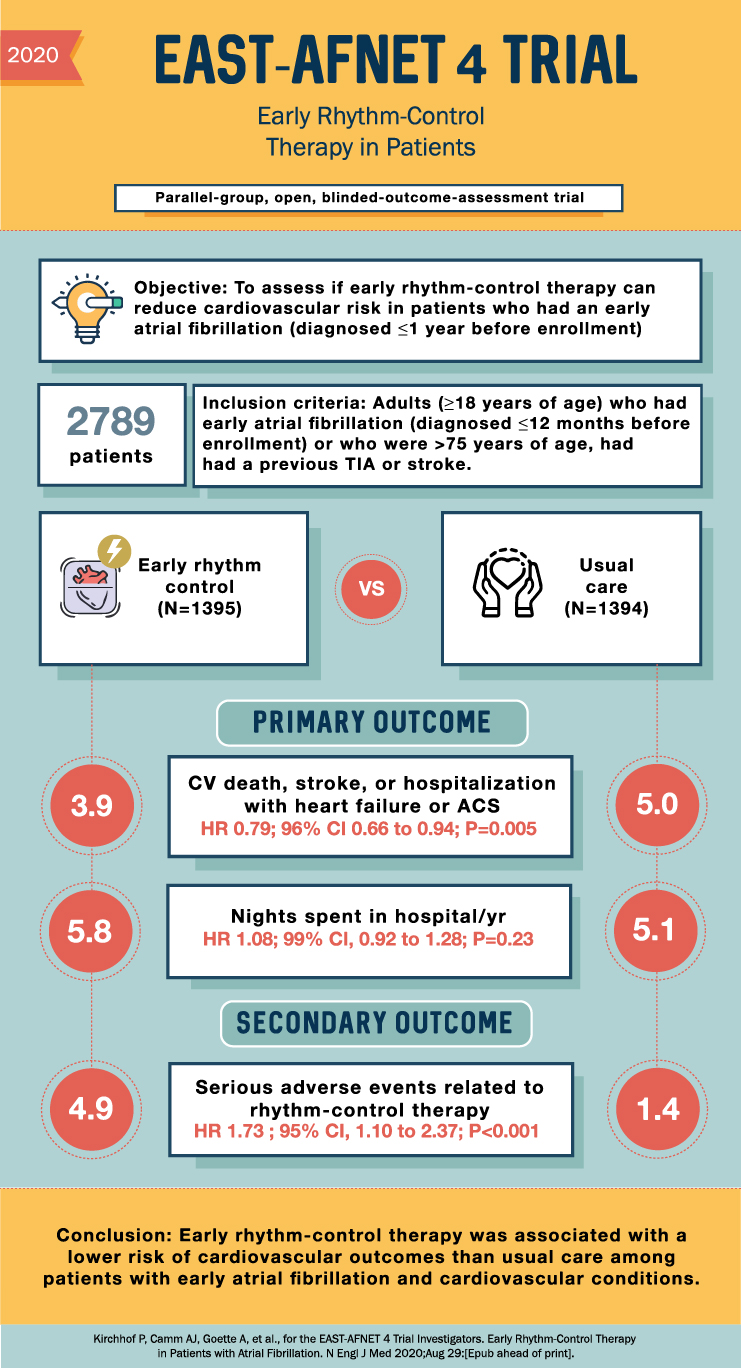
Navigating the New Era: Landmark Clinical Trials on Eliquis (Apixaban) for Anticoagulation in Atrial Fibrillation
Atrial fibrillation (AFib) is a prevalent cardiac arrhythmia that significantly elevates the risk of stroke and systemic embolism. As a result, effective anticoagulation therapy is crucial for managing AFib patients. Over the past decade, novel oral anticoagulants (NOACs) have challenged … Read More
Pioneering the Path: Key Landmark Trials on Ablation Procedures for Atrial Fibrillation
Delve into the pivotal clinical trials that have shaped our understanding and management of atrial fibrillation through ablation procedures. … Read More
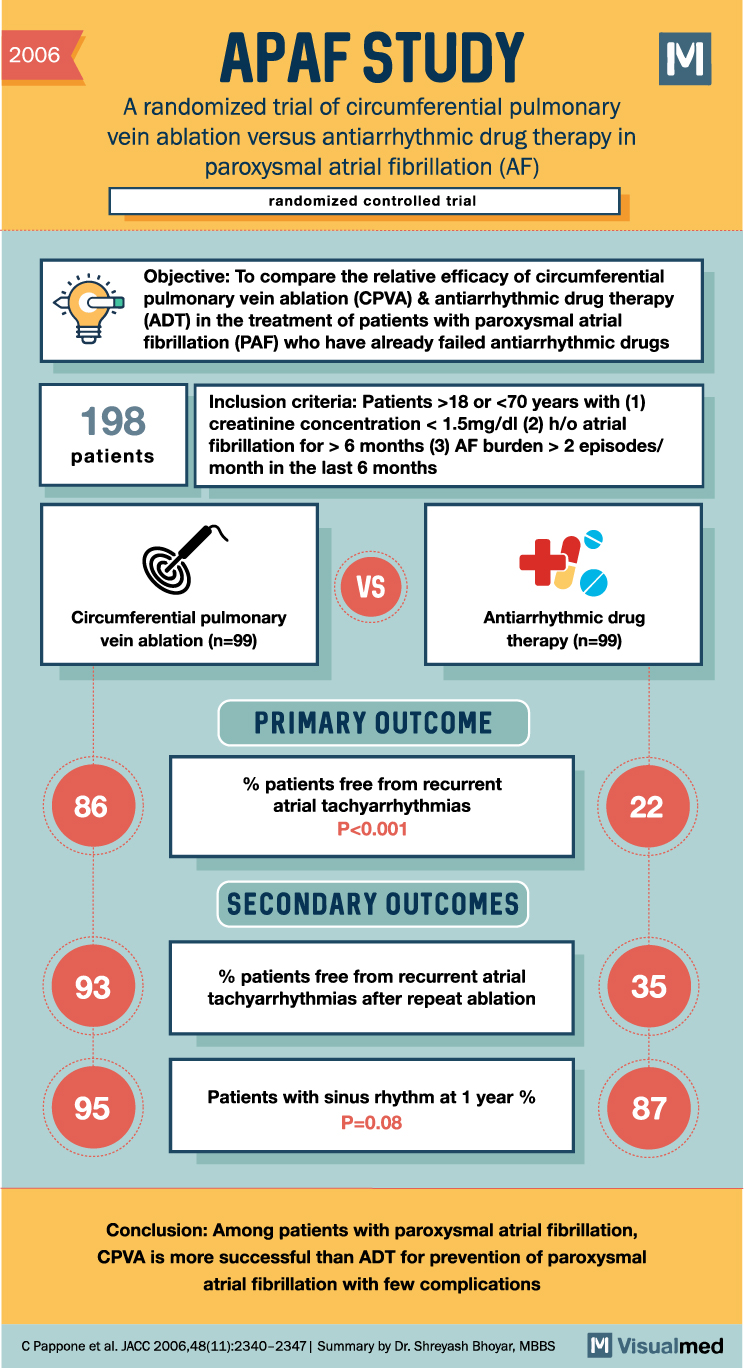
APAF Trial: Ablation or Antiarrhythmics for PAF
2006 APAF STUDY A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation (AF) randomized controlled trial M Objective: To compare the relative efficacy of circumferential pulmonary vein ablation (CPVA) & antiarrhythmic drug … Read More
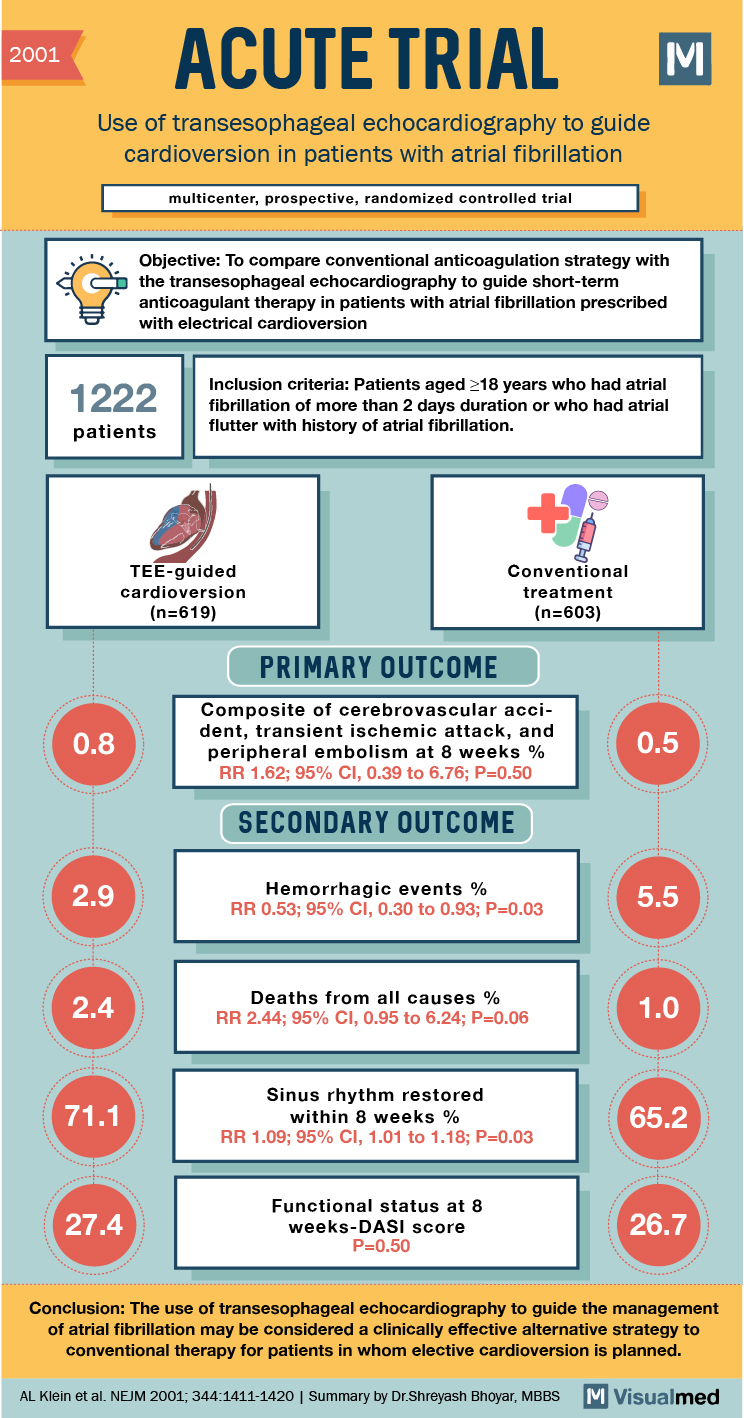
ACUTE Trial Summary: TEE-Guided Cardioversion for AFib
2001 ACUTE TRIAL Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation multicenter, prospective, randomized controlled trial Objective: To compare conventional anticoagulation strategy with the transesophageal echocardiography to guide short-term anticoagulant therapy in patients with atrial fibrillation … Read More
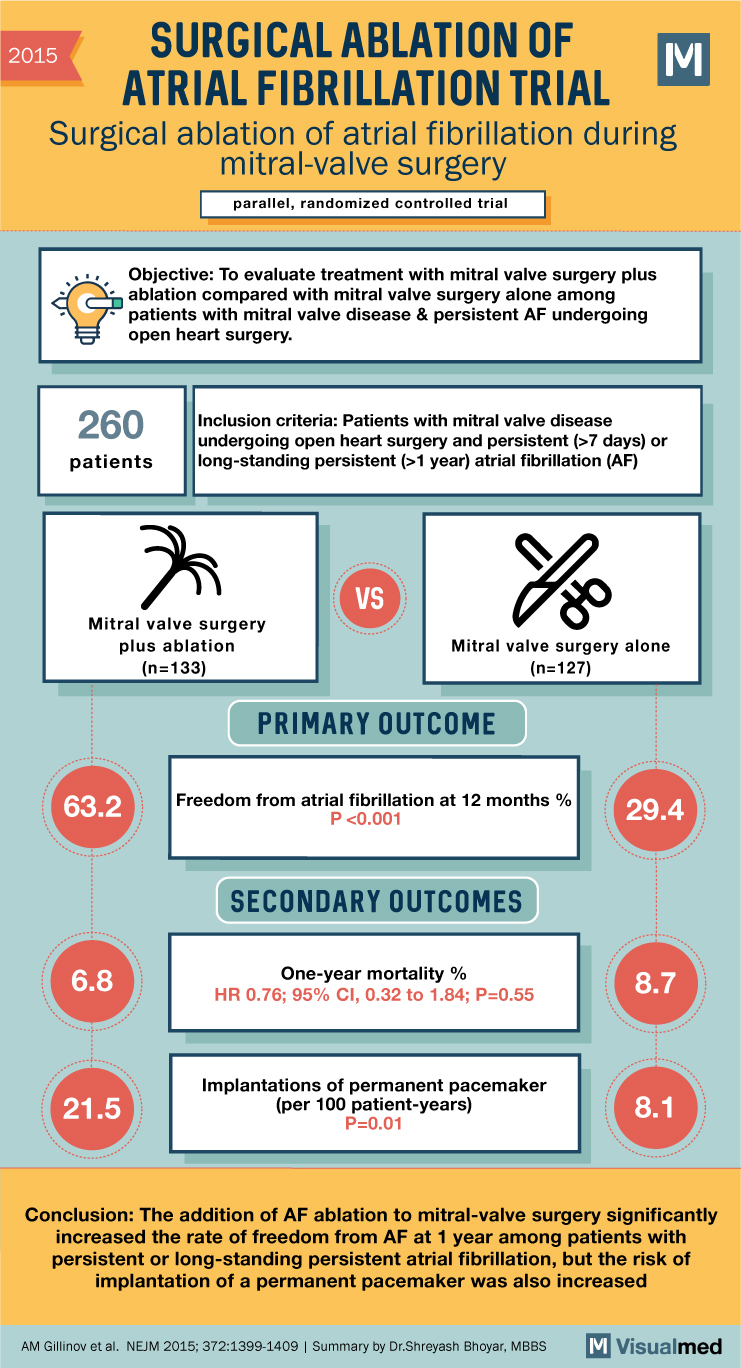
Surgical Ablation of AFib with MV Surgery
2015 SURGICAL ABLATION OF ATRIAL FIBRILLATION TRIAL Surgical ablation of atrial fibrillation during mitral-valve surgery parallel, randomized controlled trial M Objective: To evaluate treatment with mitral valve surgery plus ablation compared with mitral valve surgery alone among patients with mitral … Read More
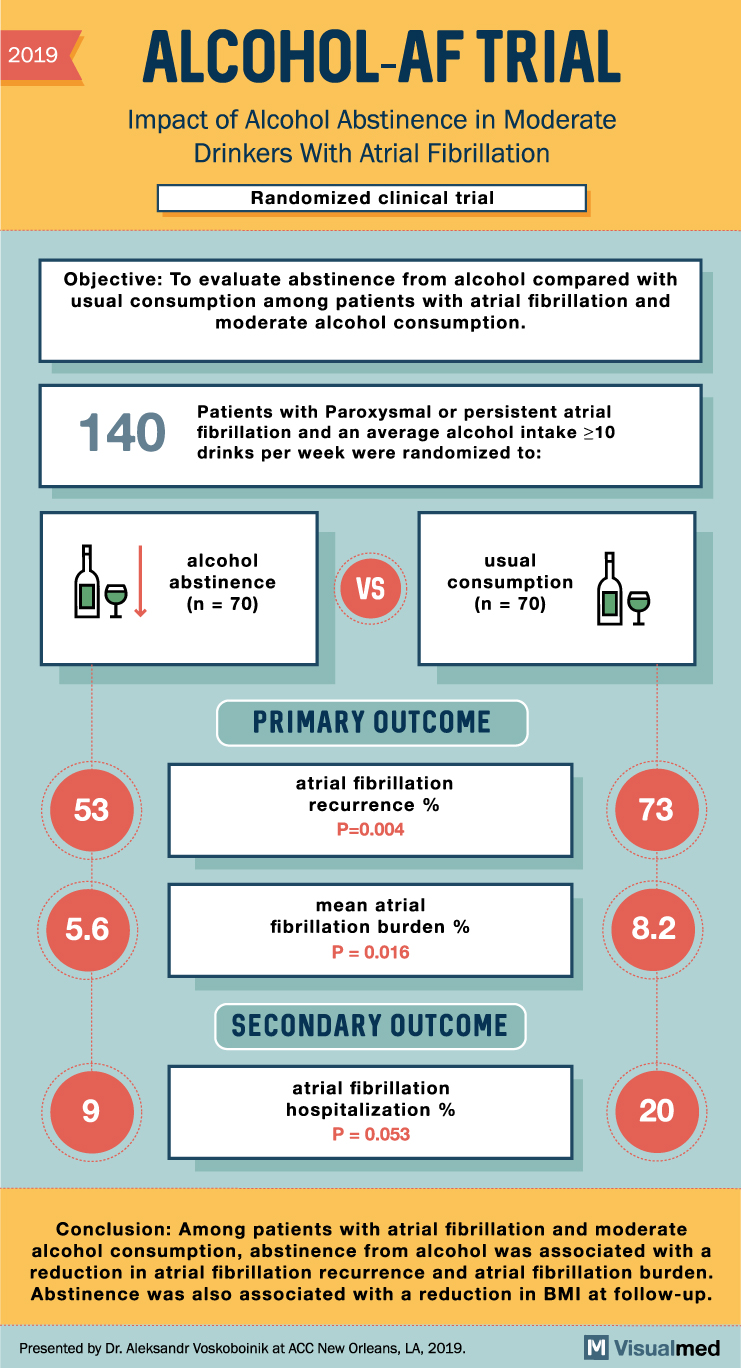
ALCOHOL-AF Trial Summary: Alcohol and AFib
2019 ALCOHOL-AF TRIAL Impact of Alcohol Abstinence in Moderate Drinkers With Atrial Fibrillation Randomized clinical trial Objective: To evaluate abstinence from alcohol compared with usual consumption among patients with atrial fibrillation and moderate alcohol consumption. 140 bel 53 5.6 9 … Read More
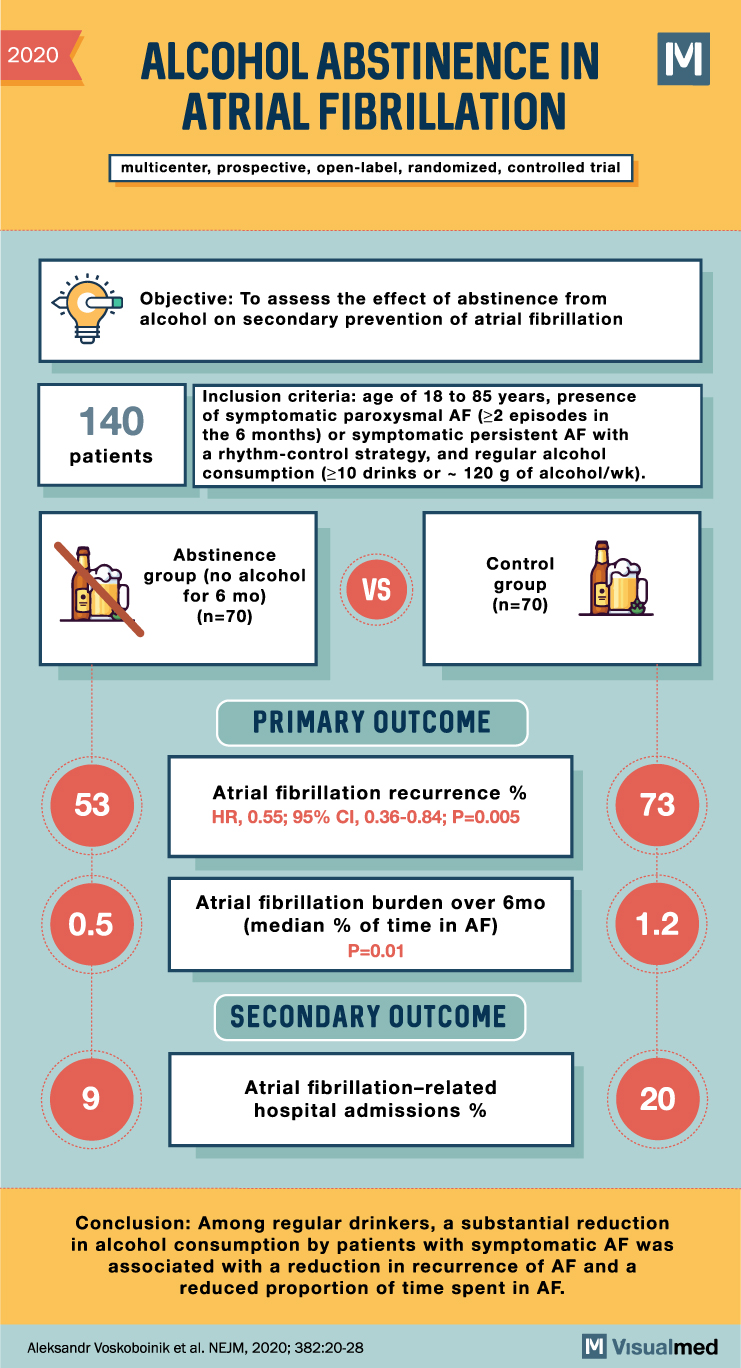
Alcohol Abstinence in AFib Clinical Trial Summary
2020 ALCOHOL ABSTINENCE IN ATRIAL FIBRILLATION multicenter, prospective, open-label, randomized, controlled trial Objective: To assess the effect of abstinence from alcohol on secondary prevention of atrial fibrillation 140 patients Inclusion criteria: age of 18 to 85 years, presence of symptomatic … Read More
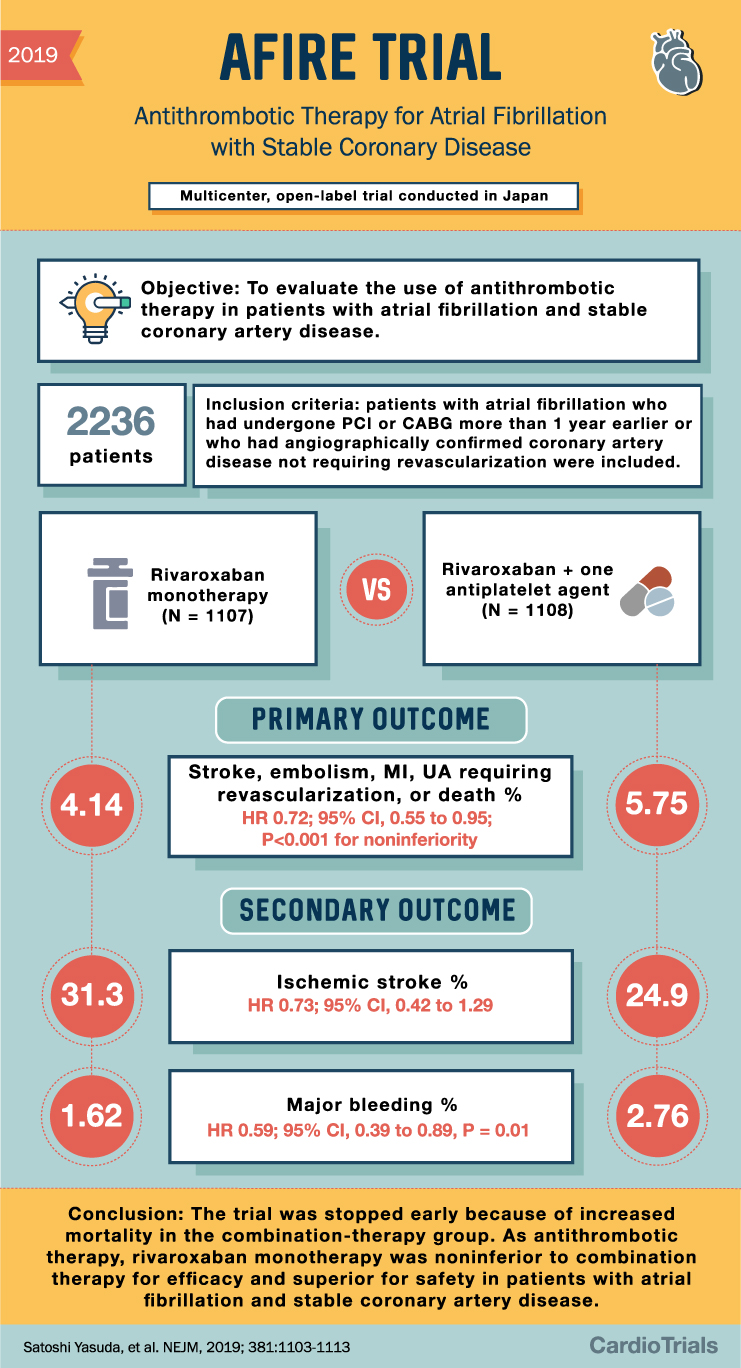
AFIRE Trial Summary: Antithrombotics in AFib and CAD
2019 AFIRE TRIAL Antithrombotic Therapy for Atrial Fibrillation with Stable Coronary Disease Multicenter, open-label trial conducted in Japan Objective: To evaluate the use of antithrombotic therapy in patients with atrial fibrillation and stable coronary artery disease. 2236 patients 4.14 Inclusion … Read More
